
Pre-Hospital Education Centre
Kevin Letchford, Clinical Education Manager & Critical Care Paramedic
When a new doctor or critical care paramedic joins Thames Valley Air Ambulance, they don’t arrive as beginners. Each one already has years of experience behind them.
But stepping into the world of pre-hospital critical care is different to the emergency room.
Our clinicians need to deliver complex medical interventions in the toughest conditions, for example a busy roadside; in people’s homes with anxious families looking on; or even in a ditch in the middle of the night.
That’s why we run our Foundations in Pre-Hospital Critical Care (FPHCC) course. I’d describe it as a springboard which helps experienced clinicians adapt their skills to the unique demands of working outside of hospital.
Part of our mission is to empower our critical care paramedics, doctors and the wider pre-hospital community with the knowledge, skills and confidence to deliver consistent and outstanding patient care through innovative education opportunities and lifelong learning.
The course takes place over four days and is designed to develop confidence and competence in managing critically ill or injured patients.
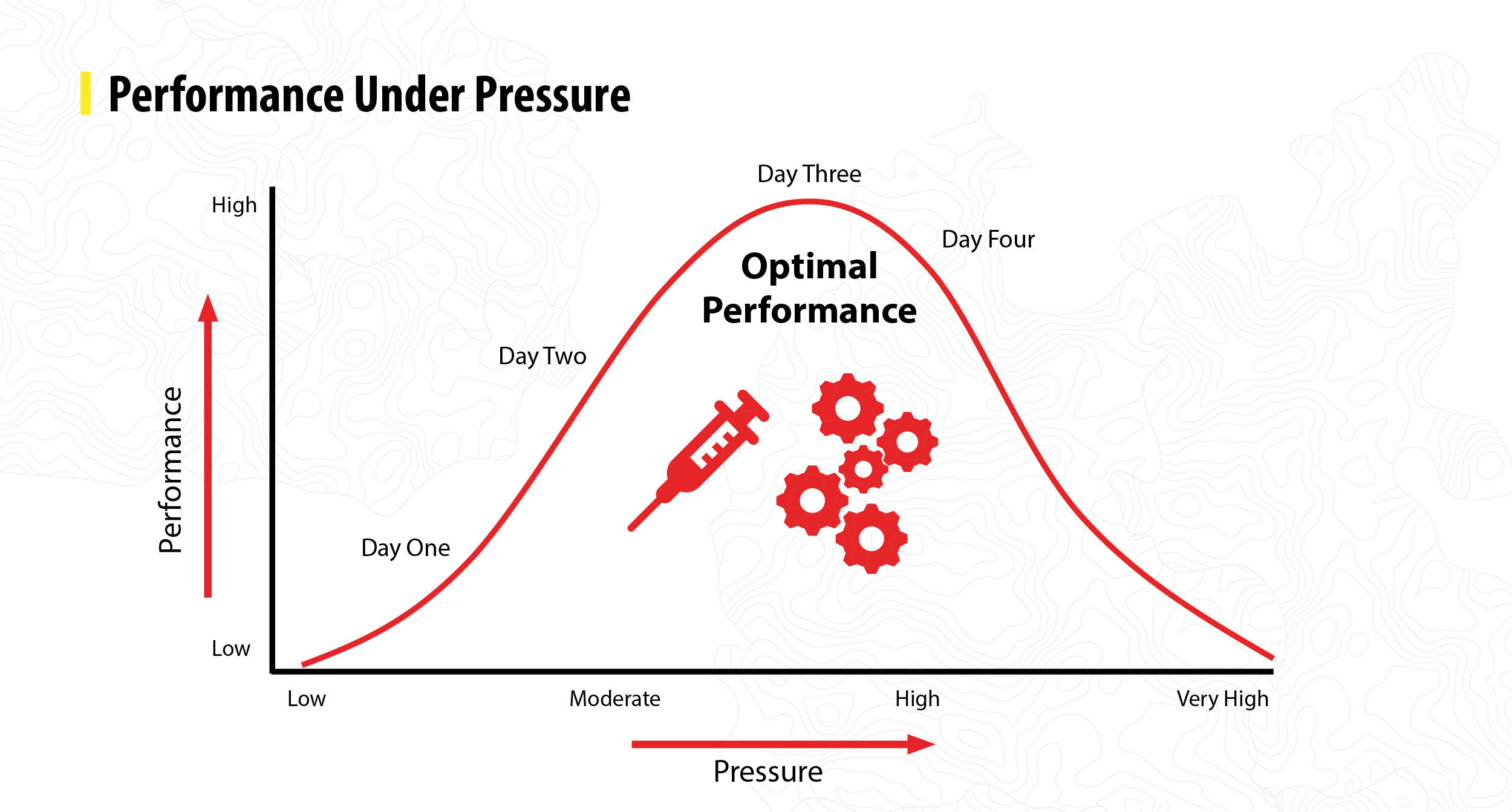
It includes a mixture of classroom-based lectures, practical skills, and simulations which replicate real emergencies. It’s carefully structured so that pressure and complexity increase from day one through to day four, following the principles of the pressure-performance curve.
What is the pressure-performance curve?
The pressure-performance curve is a bell-shaped trajectory that shows the relationship between pressure and performance.
When pressure becomes too much, people’s performance generally begins to suffer. But managed pressure is important for optimum performance – it’s why you often hear elite athletes talking about being ‘in the zone’.
In the world of Pre-Hospital Emergency Medicine (PHEM), that pressure could be the complexity of the injury or illness, the conditions you’re working in, having distressed family members nearby, or multiple distractions.
The course allows new clinicians – or ‘candidates’ – to understand how they respond to stress, helping them to develop strategies to deliver safe and effective care. By the end of the four days, candidates have experienced gradual and carefully managed journey to achieving optimal performance under pressure.
What else are we looking for from candidates?
Being able to carry out skills in hospital does not automatically translate to pre-hospital care. It’s a different skillset with unique challenges.
This course ensures everyone has a shared understanding of the challenges we face and can function as part of our tight-knit team. It’s as much about introducing our culture as it is about clinical ability.
When we evaluate candidates we’re not looking for perfection or the finished article. We fully expect them to get things wrong, because that’s how people grow and learn. The educational culture of FPHCC is designed to make it safe to do that, with teaching and collaborative learning at the heart of it.
Of course, clinical knowledge and skills are vital, but what we’re also looking for is candidates to demonstrate clear thinking, safe decision-making, and the ability to bring the team with them. The people who stand out are those who stay calm under pressure, communicate well, and adapt when things don’t go to plan.

So, how do we put people in situations where they’re learning, but also showing us how they cope under pressure?
The key is to build the pressure gradually.
Day one begins in the classroom, where we introduce the principles of Pre-Hospital Emergency Medicine. PHEM demands more than just clinical skills, it also requires the ability to lead, adapt, and make critical decisions in unpredictable, complex, and resource-limited environments. Candidates also explore how human factors, and coordination with other emergency services can shape the outcome.
On day two, it’s time to put the theory into practice. Candidates have an opportunity to perform surgical procedures we describe as high acuity, low occurrence or ‘HALO’. These include thoracostomy, thoracotomy, surgical airways and the emergency delivery of a baby – interventions which are rare but high-stakes, carried out under high stress situations, when every minute matters.

It’s then time to ramp up the pressure. Day three has the candidates traveling offsite to take part in multiple scenarios designed to replicate real emergencies.
There’s no telling what our crew could face on any given day, so our clinicians need to be ready for any eventuality. We use real data to design scenarios based on call outs they might expect to face within our region. For example, we have over 200 miles of motorway throughout Berkshire, Buckinghamshire and Oxfordshire so we’re regularly called to serious road traffic collisions.
One of the toughest tests this year was exactly that, a scenario where a car collided with a cyclist.
As the candidates arrive at the incident, ambulance paramedics are already on scene helping the patient. The patient is critically unwell and in need of urgent treatment, including pre-hospital blood transfusion.
From a clinical perspective, we’re looking for the candidates to demonstrate safe, structured decision-making, sound clinical judgement under pressure, and the ability to prioritise interventions effectively. We’re looking for high-quality patient care alongside clear communication with the whole team. It’s no easy task.
But as the scenario develops, there’s more than meets the eye.
The driver of the vehicle – clearly intoxicated – is acting frantic and disruptive, adding to the chaos. While our candidates focus their efforts on saving the patient’s life, a cry is heard from a nearby bystander: “there’s another cyclist!” The stark reality emerges that the driver struck not one cyclist but two, with the second casualty obscured by a hedgerow.
This sudden escalation raises the complexity of the scenario, increasing the pressure and forcing candidates to make rapid and difficult triage decisions.

Where possible, we use trained actors to play patients and bystanders. This helps to bring a level of authenticity to each scenario, replicating the emotions, tensions, and chaos of a real emergency.
This is perhaps most evident in one of the afternoon scenarios involving an intentional self-harm where the patient is found by her distressed partner.
Although it’s a simulation, it’s difficult for everyone involved. The realism of the scenario, combined with its emotional weight, can be challenging for candidates, crew, and observers alike.
The experience highlights not only the technical and clinical expertise required for the role, but also the emotional resilience required to manage situations that are both complex and distressing.
It’s precisely this realism, delivered in a safe learning environment, that makes these scenarios a powerful educational tool, preparing clinicians to face the realities of pre-hospital care with skill, composure, and compassion.
Last year, our crew were dispatched to 155 incidents involving intentional self-harm, so it’s sadly the sort of thing our crew could experience in a real emergency.

Each scenario is designed to stretch them. This is where the safety net comes in – the debriefs.
After each scenario a debrief takes place. They help turn those pressure moments into valuable lessons and that is where the real learning happens.
We have a structured model that we all follow, so the process is consistent, constructive and supportive. Each debrief focuses on three things: areas of strength, areas for improvement, and individual learning points that candidates can carry forward.
A big part of our educational culture is making it a genuinely safe space. We expect people to make mistakes; that’s part of the learning journey. It’s about growth, not criticism.
We also give candidates the space to reflect on how they felt in the moment whether they were calm, under pressure, or aware of their team’s needs. That emotional insight is just as valuable as clinical knowledge.

Delivering the course is a massive team effort.
What humbles me most is how people from across the charity and beyond want to be involved. It’s not every day that you see a senior medical director with a mop and bucket, helping to keep the environment safe; or, a volunteer acting as a concerned bystander. But that really captures the spirit of this course – no job is too small if it keeps things on track and creates the right learning space.
This team effort culminates on the final day, where candidates are joined by colleagues from the ambulance service and fire service to simulate a multi-agency response to a major road traffic collision.

The course is deliberately designed so that pressure builds step by step. We start with core principles and straight-forward scenarios, then add layers of complexity until candidates find themselves managing multiple patients in chaotic, unpredictable environments.
The goal isn’t to break anyone or push them to boiling point. It’s about showing them what they can achieve under pressure.
Our clinicians never know what the next call out might bring, but through our Foundations in Pre-Hospital Critical Care course they discover that with the right skills, teamwork and mindset they can rise to the challenge.
The course isn’t the end of their journey, it’s just the beginning. From here, candidates move into supervised shifts, ongoing mentorship, and further training. But FPHCC gives them their first taste of what it means to deliver critical care under pressure in unfamiliar environments, and the confidence to take that next step.

12/01/2026

News
02/12/2025

Blog
08/08/2025

News
21/07/2025

News
Join the community by signing up and keep up to date with news and events.
Our website makes use of the following types of cookies:
| Cookie | Duration | Description |
|---|---|---|
| __cflb | 1 hour | The __cflb cookie allows Cloudflare to return an end user to the same customer origin for a specific period of time configured by the customer. This allows the end user to have a seamless experience (for example, this cookie is used for keeping an end user’s items in a shopping cart while they continue to navigate around the website). This cookie is a session cookie that lasts from several seconds up to 24 hours. This is a first party cookie. |
| salt_recent_events | 1 month | This cookie monitors which event pages the user has visited, in order to provide them a list of recently visited event pages. This cookie is only used to improve the user's experience of our website. This is a first party cookie. |
| salt_recent_post | 1 month | This cookie monitors which web stories the user has read, in order to provide them a list of recently read stories. This cookie is only used to improve the user's experience of our website. This is a first party cookie. |
| yt-remote-cast-installed | session | The yt-remote-cast-installed cookie is used to store the user's video player preferences using embedded YouTube video. This is a third party cookie |
| yt-remote-connected-devices | session | YouTube sets this cookie to store the user's video preferences using embedded YouTube videos. This is a third party cookie. |
| yt-remote-device-id | session | YouTube sets this cookie to store the user's video preferences using embedded YouTube videos. This is a third party cookie. |
| yt-remote-fast-check-period | session | The yt-remote-fast-check-period cookie is used by YouTube to store the user's video player preferences for embedded YouTube videos. This is a third party cookie. |
| yt-remote-session-app | session | The yt-remote-session-app cookie is used by YouTube to store user preferences and information about the interface of the embedded YouTube video player. This is a third party cookie. |
| yt-remote-session-name | session | The yt-remote-session-name cookie is used by YouTube to store the user's video player preferences using embedded YouTube video. This is a third party cookie. |
| ytidb::LAST_RESULT_ENTRY_KEY | session | The cookie ytidb::LAST_RESULT_ENTRY_KEY is used by YouTube to store the last search result entry that was clicked by the user. This information is used to improve the user experience by providing more relevant search results in the future. This is a third party cookie. |
| Cookie | Duration | Description |
|---|---|---|
| __Secure-ROLLOUT_TOKEN | 6 months | Is used by YouTube to manage the phased rollout of new features and updates. This cookie helps assign users to specific test groups for experimental features, such as changes to the user interface or video player. The __Secure- prefix indicates that the cookie is only transmitted over a secure HTTPS connection, enhancing data security. This is a third party cookie. |
| _ga | 2 years | This cookie is installed by Google Analytics. This cookie is used to calculate visitor, session, campaign data and keep track of site usage for the site's analytics report. This cookie store information anonymously and assign a randomly generated number to identify unique visitors. This is a first party cookie. |
| _ga_* | 1 year 1 month 4 days | Google Analytics sets this cookie to store and count page views. This is a first party cookie. |
| _gat_gtag_UA_* | 1 minute | Google Analytics sets this cookie to store a unique user ID. This is a first party cookie. |
| _gat_gtag_UA_77930033_1 | 1 minute | This cookie is used by Google Tag Manager to store and track website conversions. This is a first party cookie. |
| _gcl_au | 3 months | Google Tag Manager sets the cookie to experiment advertisement efficiency of websites using their services. This is a third party cookie. |
| _gid | 1 day | This cookie is installed by Google Analytics. The cookie is used to store information of how visitors use a website and helps in creating an analytics report of how the wbsite is doing. The data collected including the number visitors, the source where they have come from, and the pages viisted in an anonymous form. This is a first party cookie. |
| _hjAbsoluteSessionInProgress | 30 minutes | This cookie is used by Hotjar to detect the first pageview session of a user. This is a True/False flag set by the cookie. This is a third party cookie. |
| _hjFirstSeen | 30 minutes | This is set by Hotjar to identify a new user’s first session. It stores a true/false value, indicating whether this was the first time Hotjar saw this user. It is used by Recording filters to identify new user sessions. This is a third party cookie. |
| _hjid | 1 year | This cookie is set by Hotjar. This cookie is set when the customer first lands on a page with the Hotjar script. It is used to persist the random user ID, unique to that site on the browser. This ensures that behavior in subsequent visits to the same site will be attributed to the same user ID. This is a third party cookie. |
| _hjIncludedInPageviewSample | 30 minutes | This cookie is set to let Hotjar know whether a visitor is included in the data sampling defined by our site's pageview limit. This is a third party cookie. |
| _hjIncludedInSessionSample | 2 minutes | This cookie is set to let Hotjar know whether a visitor is included in the data sampling defined by the website's daily session limit. This is a third party cookie. |
| _hjSession_* | 1 hour | Hotjar sets this cookie to ensure data from subsequent visits to the same site is attributed to the same user ID, which persists in the Hotjar User ID, which is unique to that site. This is a first party cookie. |
| _hjSessionUser_* | 1 year | Hotjar sets this cookie to ensure data from subsequent visits to the same site is attributed to the same user ID, which persists in the Hotjar User ID, which is unique to that site. This is a first party cookie. |
| _hjTLDTest | session | This cookie is set by HotJar. When the Hotjar script executes they try to determine the most generic cookie path to use, instead of the page hostname. This is done so that cookies can be shared across subdomains (where applicable). To determine this, HotJar try to store the _hjTLDTest cookie for different URL substring alternatives until it fails. After this check, the cookie is removed. This is a third party cookie. |
| _uetsid | session | Bing Ads sets this cookie to engage with a user that has previously visited the website. This is a third party cookie. |
| _uetvid | session | Bing Ads sets this cookie to engage with a user that has previously visited the website. This is a third party cookie. |
| VISITOR_INFO1_LIVE | 5 months 27 days | This cookie is set by Youtube. Used to track the information of the embedded YouTube videos on a website. This is a third party cookie. |
| vuid | 1 year 1 month 4 days | Vimeo installs this cookie to collect tracking information by setting a unique ID to embed videos on the website. This is a third party cookie. |
| YSC | session | This cookie is set by Youtube and is used to track the views of embedded videos. This is a third party cookie. |
| Cookie | Duration | Description |
|---|---|---|
| _fbp | 3 months | This cookie is set by Facebook to deliver advertisement when they are on Facebook or a digital platform powered by Facebook advertising after visiting this website. This is a first party cookie. |
| fr | 3 months | The cookie is set by Facebook to show relevant advertisments to the users and measure and improve the advertisements. The cookie also tracks the behavior of the user across the web on sites that have Facebook pixel or Facebook social plugin. This is a third party cookie. |
| IDE | 1 year 24 days | Used by Google DoubleClick and stores information about how the user uses the website and any other advertisement before visiting the website. This is used to present users with ads that are relevant to them according to the user profile. This is a third party cookie. |
| NID | 6 months | Google sets the cookie for advertising purposes; to limit the number of times the user sees an ad, to unwanted mute ads, and to measure the effectiveness of ads. This is a first party cookie. |
| test_cookie | 15 minutes | This cookie is set by doubleclick.net. The purpose of the cookie is to determine if the user's browser supports cookies. This is a third party cookie. |
| VISITOR_PRIVACY_METADATA | 6 months | YouTube sets this cookie to store the user's cookie consent state for the current domain. This is a third party cookie. |
| yt.innertube::nextId | session | YouTube sets this cookie to register a unique ID to store data on what videos from YouTube the user has seen. This is a third party cookie. |
| yt.innertube::requests | session | YouTube sets this cookie to register a unique ID to store data on what videos from YouTube the user has seen. This is a third party cookie. |